what is the pathophysiology of hypertensive emergency evidence based
Hypertensive emergency (HE) is characterized by a significant and acute increase in blood pressure leading to acute target-organ damage. The pathophysiology of hypertensive emergency is complex and multifactorial. Here is an evidence-based summary of the key mechanisms involved:
-
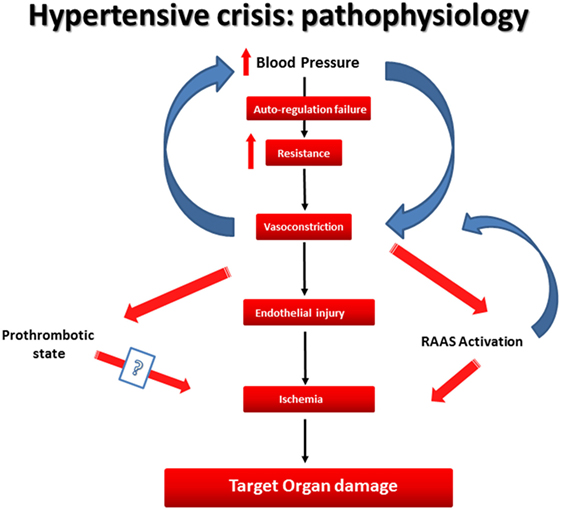
Vascular Resistance and Autoregulation: One central aspect of the pathophysiology of hypertensive emergencies involves an abrupt increase in systemic vascular resistance. This resistance often results from the activation of the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system stimulation. According to an article from PMC, the body's autoregulatory mechanisms become impaired, leading to significant fluctuations in blood pressure (source). The failure of these regulatory processes to compensate for sudden anthropometric changes can lead to a severe hypertensive crisis.
-
Endothelial Dysfunction: Increased blood pressure typically inflicts damage on the endothelium, the inner lining of blood vessels. This injury manifests as endothelial dysfunction, which contributes to additional vasoconstriction and vascular permeability changes. The impaired release of vasodilators such as nitric oxide (NO) exacerbates elevated vascular tone, resulting in further increases in blood pressure (source).
-
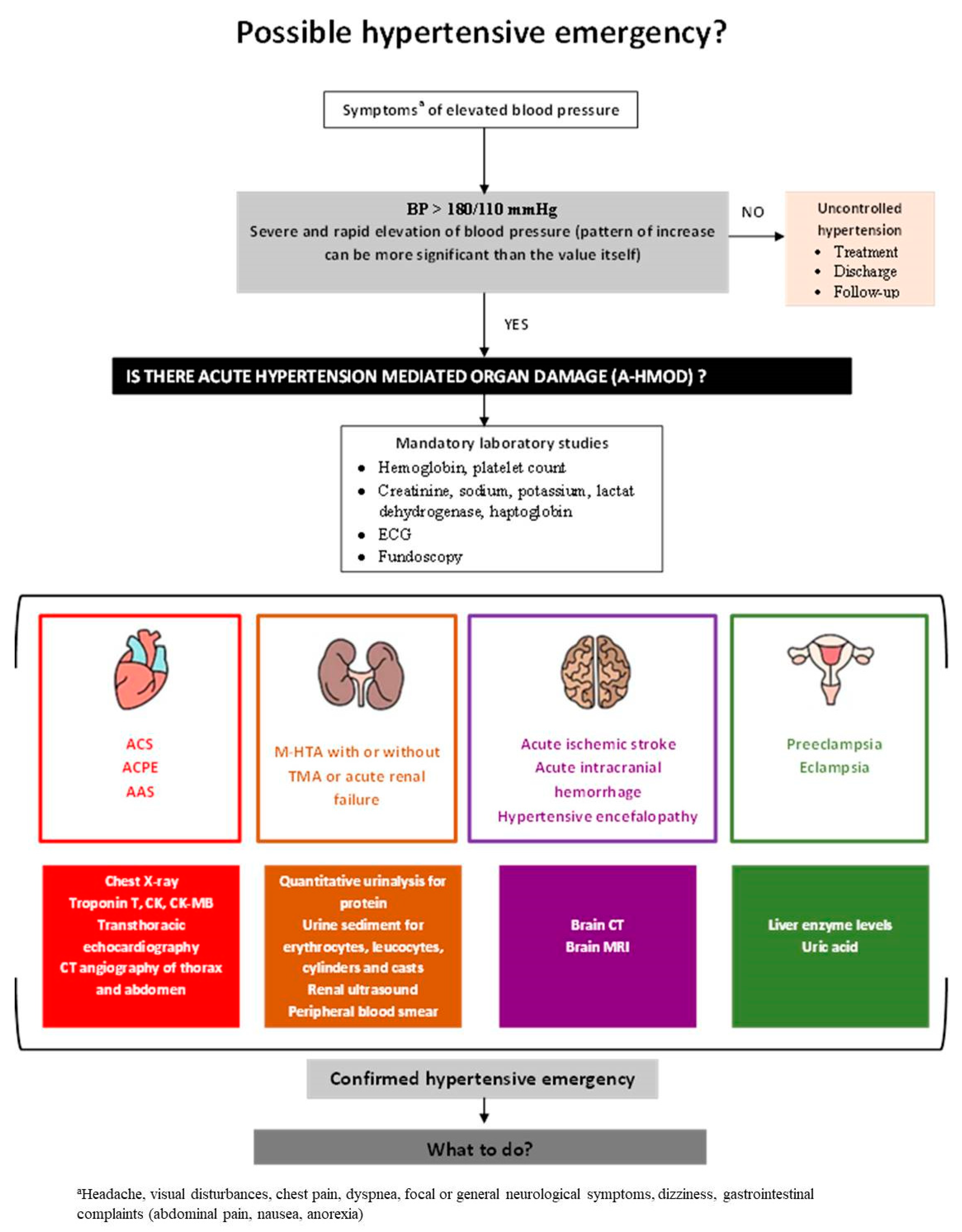
Organ Damage: As blood pressure rises, it can initiate a cascade of events leading to target organ damage in systems such as the cardiovascular, renal, and nervous systems. The Journal of the American Heart Association outlines how chronic hypertension leads to hypertensive-mediated organ damage, primarily affecting the brain (stroke), heart (myocardial infarction), and kidneys (acute kidney injury) (source). The resultant ischemia from severely elevated blood pressure can lead to tissue necrosis and dysfunction.
-
Neurohormonal Activation: Significant elevations in blood pressure trigger an overactivation of neurohormonal systems, including catecholamines (e.g., epinephrine and norepinephrine) and various vasoconstrictor peptides. This neurohormonal response aims to compensate for the perceived low perfusion states, leading to a further increase in heart rate and vascular resistance (source).
-
Acute Medical Events and Stressors: The transition from chronic to acute hypertension often correlates with acute medical events, such as myocardial infarction, severe anxiety, or illicit drug use (e.g., cocaine), which can precipitate sudden and severe elevations in blood pressure (source). Factors that contribute to this transition involve physical and emotional stressors that activate the sympathetic nervous system, resulting in significant increases in vascular resistance.
In summary, the pathophysiology of hypertensive emergencies is characterized by a combination of systemic vascular resistance increases, endothelial damage, neurohormonal activation, and organ damage from elevated blood pressure. Understanding these mechanisms aids in formulating treatment strategies to address acute hypertensive crises effectively.
Sources
Related Questions
Work fast from anywhere
Stay up to date and move work forward with BrutusAI on macOS/iOS/web & android. Download the app today.
