What does United Healthcare mean by "step therapy" for a
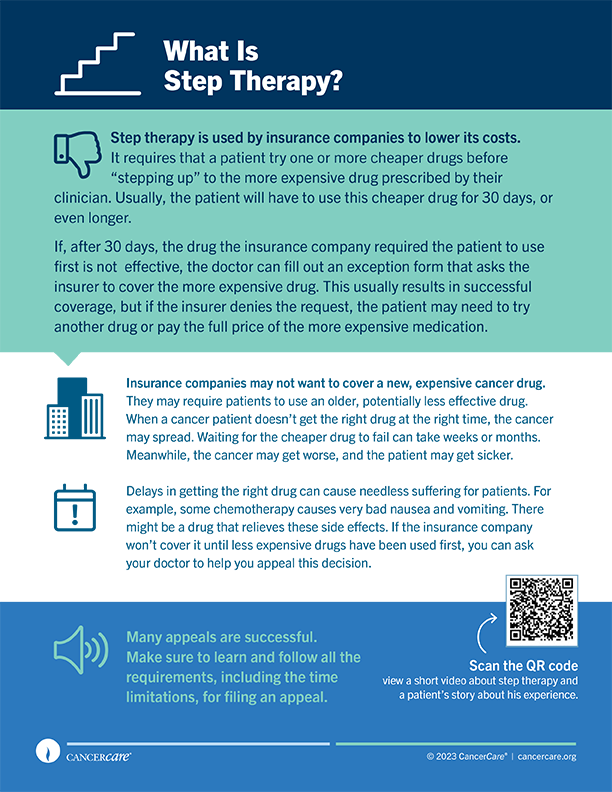
"Step therapy" as defined by United Healthcare refers to a prior authorization process for medications where patients are initially required to try and fail on one or more preferred (often less expensive) medications before moving on to more costly alternatives. This approach is intended to ensure that patients receive the most effective and cost-efficient treatments for their medical conditions.
The step therapy process typically begins with the prescribing physician detailing the medical necessity for the prescribed medication. United Healthcare assesses this information to determine whether the requested medication will be covered under the patient's plan. If a medication is approved via the step therapy protocol, coverage will generally be authorized for a period of 12 months, as specified in their policies.
For further information regarding the specifics of step therapy and how it may impact treatment decisions, you can refer to resources provided by United Healthcare, such as their Pharmacy Benefits FAQs and Medicare Part B step therapy programs. Additionally, the Centers for Medicare & Medicaid Services outlines broader definitions and implications of step therapy through their official guidance.
In summary, step therapy promotes the use of preferential treatments before progressing to more expensive options, thereby aligning treatment approaches with cost-effectiveness while still addressing patient needs through thorough medical justification.
Sources
Related Questions
Work fast from anywhere
Stay up to date and move work forward with BrutusAI on macOS/iOS/web & android. Download the app today.
